Chapter 2
Experience of patients and access to treatment
2.1
As outlined in Chapter 1, the committee has received over 1000 personal
submissions from or on behalf of Australians suffering from chronic
debilitating symptoms. The committee is deeply concerned by evidence that many
submitters have experienced significant challenges in accessing appropriate
healthcare to address their symptoms. In particular the committee is concerned by
evidence that suggests submitters have been insulted and humiliated by some
medical practitioners when seeking treatment.
2.2
This chapter examines the experience of submitters in accessing
treatment, particularly those diagnosed with Lyme-like illness. It examines how
the ongoing debate about whether Lyme disease is endemic to Australia
contributes to the perceived stigma about diagnoses of Lyme-like illness and
impacts on the ability of patients to access treatment. It also examines the
treatments prescribed by Lyme-literate practitioners and allegations that these
practitioners are unfairly targeted for disciplinary action by medical
authorities.
Experience of sufferers of chronic debilitating symptoms
2.3
Submitters suffering chronic debilitating symptoms can be divided into four
main groups:
-
those who acquired and were diagnosed with classical Lyme disease
in an endemic area overseas;
-
those who acquired their illness overseas but weren't diagnosed;
-
those who became ill following a tick or other insect bite in
Australia; and
-
those who have experienced a long-term chronic illness in
Australia and may or may not have been bitten by a tick or other insect.
2.4
The common experiences of patients in these groups are summarised below.
Illness acquired overseas
2.5
A small number of submitters explained that they acquired their illness overseas.
In some cases, patients became ill following a tick bite in an area where
classical Lyme disease is endemic.[1]
In other cases, patients do not recall a tick bite, but became ill following
another kind of bite (such as bed-bugs).[2]
A number of submitters do not recall any kind of bite and their symptoms did
not manifest until after returning to Australia.[3]
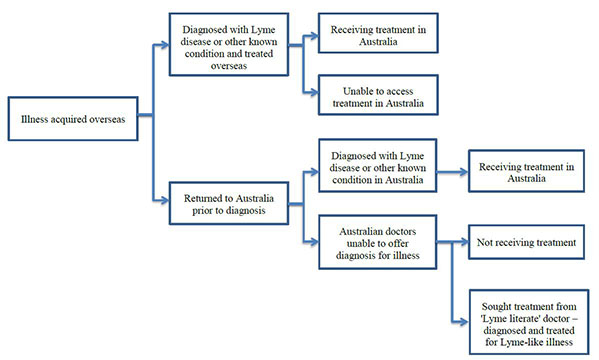
The common treatment pathways for these submitters are illustrated in Figure 2.1.
Figure 2.1 – Patient treatment pathways –Illness acquired overseas
Illness acquired in Australia
2.6
The majority of submitters stated that they acquired their illness in
Australia. In many cases submitters had no history of travel to an endemic area
for classical Lyme disease.
Illness following tick bite
2.7
Some submitters state that they became ill immediately following a tick
bite in Australia. Symptoms described by these submitters include a rash around
the bite and a range of symptoms including fatigue, arthritis and chronic pain.[4]
2.8
In some cases, submitters were diagnosed with other known tick-borne
infections, such as Q fever, Spotted Fever, Rickettsia, Queensland Tick Typhus
or allergy to tick toxin, and received treatment.[5]
2.9
However, in most cases, the submitters state that medical practitioners
were not able to identify or diagnose the illness, or offer any effective treatment.[6]
Long-term chronic illness
2.10
The largest group of submitters is those who have experienced a
long-term chronic illness. In many cases, these submitters cannot recall being
bitten by a tick. In cases where submitters can recall a tick bite, this may
have predated the onset of their illness by a number of years.[7]
2.11
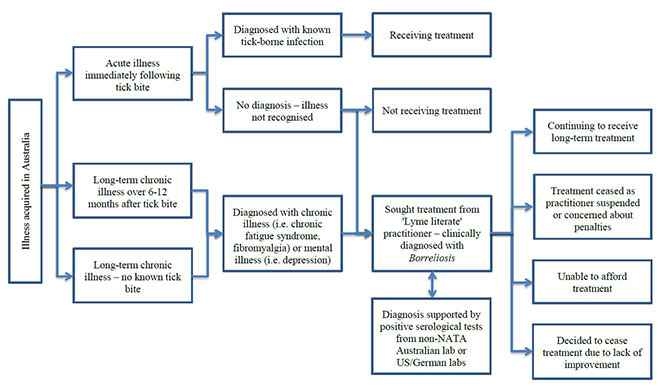
Figure 2.2 outlines the treatment pathways for these submitters.
Figure 2.2 – Patient treatment pathways from submissions – Illness acquired
in Australia
Treatment for patients
2.12
The committee heard that patients diagnosed with chronic debilitating
symptoms experience significant difficulties accessing diagnosis and treatment
from Australian healthcare services.
Illness acquired overseas
2.13
Submitters who acquired their illness overseas expressed particular
concern that Australian medical practitioners may not recognise or effectively
diagnose overseas illnesses, such as classical Lyme disease.
2.14
The committee heard that as part of the Chief Medical Officer's Clinical
Advisory Council on Lyme Disease, the department has been working with states
and territories to raise awareness and assist with the diagnosis of classical
Lyme disease through the development of the Australian guideline on the
diagnosis of overseas acquired Lyme disease/borreliosis. Dr Gary Lum from
the Department of Health (department) told the committee:
This guide was developed with the assistance of patient
advocates as well as experts in immunology, microbiology and infectious
diseases. The guideline was shared with Australian general practitioners,
emergency physicians, other relevant specialists as well as the Australian
Medical Association.[8]
2.15
However, evidence from some submitters with a history of travel to an
area where classical Lyme disease is endemic suggested that some Australian
doctors may not be aware of Lyme disease and the appropriate methods for
diagnosis and treatment. For example, one submitter noted that he acquired Lyme
disease in the United States (US) following a tick bite and was diagnosed and
treated by US doctors. Upon returning to Australia, he continued to experience
symptoms but struggled to get appropriate treatment:
For me the issue was not so much that the disease was active,
it was that doctors were unable to understand the left over side effects that
continue to deteriorate my general health and well-being ... I would love to see
more education and awareness about Lymes disease here in Australia,
particularly around managing the ongoing side-effects.[9]
2.16
Similarly, another submitter who was bitten by a tick in the US
expressed frustration at not being treated for Lyme disease in Australia:
People say being diagnosed with cancer is very scary, but try
being diagnosed with a potentially fatal disease when there is no help from the
medical profession nor support from the Government.
Regardless if the Lyme bacteria is in Australia or not, I was
bitten in the USA, so why shouldn’t I be treated? People who contact Malaria or
tuberculosis overseas can receive treatment in Australia.[10]
2.17
Dr Lum told the committee that despite efforts by the department to
educate practitioners, there was a risk that people infected with classical
Lyme disease overseas may not be appropriately treated in Australia:
We recognise that people infected overseas who return to
Australia have a risk that their classical Lyme disease will not be recognised
or appropriately treated, in spite of our regular advice to Australia's doctors
to pay attention to this situation.[11]
2.18
Dr Lum noted that the department was committed to education and
awareness raising of classical Lyme disease, but acknowledged it could do more
to communicate with the medical profession:
What the department has been trying to do is communicate with
the medical profession. If, as part of the Senate inquiry and as part of the
recommendation, we could possibly do more to communicate with the medical
profession on this, we certainly would.[12]
Illness acquired in Australia
2.19
More commonly, submitters have acquired their illness in Australia, but have
not been able to be readily diagnosed and treated by Australian medical
practitioners.
2.20
As discussed in Chapter 1, many of these submitters have been diagnosed
with Lyme disease or Lyme-like illness by 'Lyme literate' practitioners.
However, due to the significant debate in Australia about the existence of Lyme
disease, these submitters noted that they have experienced significant
challenges in accessing treatment in Australia.
The Lyme disease debate in
Australia
2.21
The existence of Lyme disease in Australia is highly controversial and
has attracted significant media attention and public debate. This debate
relates to two closely related questions:
-
whether the causative agent for classical Lyme disease (either
known Borrelia species such as B. burgdorferi or an as yet
unidentified Borrelia species) is endemic to Australia (i.e. has been
identified in Australia); and
-
consistent with the international debate about 'chronic' Lyme
disease, whether the chronic debilitating symptoms experienced by Australian
patients are caused by an ongoing active infection of Borrelia and
associated co-infections, or another as yet unidentified underlying cause or
causes.
Is classical Lyme disease endemic
to Australia?
2.22
The position of Australian Commonwealth, state and territory governments
and medical authorities is that the causative agent for classical Lyme disease
is not endemic to Australia.[13]
In their submissions to the inquiry, these authorities state that there is no
evidence to suggest that B. burgdorferi or any other Borrelia
species known to cause Lyme disease have been identified in Australian ticks or
patients.[14]
In his 2014 progress report on Lyme disease in Australia, the Chief Medical
Officer (CMO), Professor Chris Baggoley, stated that there is no evidence that
the bacteria causing Lyme disease are endemic to Australia:
There is still no routine finding of Borrelia spp in
ticks in Australia.
The conclusive finding of a bacterium that could cause Lyme
disease-like syndrome in Australia has yet to be made. Such a finding would put
beyond doubt the existence of Lyme disease, or a Lyme disease-like syndrome in
Australia.[15]
2.23
Most submissions from medical authorities[16]
support the Royal College of Pathologists Australasia (RCPA) position paper on
diagnostic testing for Lyme disease in Australia that states that:
Only a genuine case in a non-travelling Australian patient
would confirm the disease as being present in Australia.[17]
2.24
The CMO has stated that other 'vectors and routes of transmission are
postulated, but yet to be demonstrated'.[18]
In evidence to the committee, Dr Gary Lum noted that there may be a range of
possible causes for Lyme-like illness:
In the context of evolving Australian research data, we need
to consider that the cause may not be limited to a single bacterial species.
Parasitic and viral causes, as well as environmental toxins, should also be
considered for investigation, as well as other potential medical explanations.[19]
2.25
The first Australian cases of a syndrome consistent with Lyme
disease were reported in the Hunter Valley region of NSW in 1982. Further
clinical cases were reported on the NSW south and central coast in 1986, and in
Queensland between 1986 and 1989.[20]
Since these cases, there have been a number of studies examining whether
locally acquired Lyme disease exists in Australia. According to a recent paper
summarising research into Lyme disease in Australia, these studies have found
no conclusive evidence that indicates the presence of the causative agent for
Lyme Disease—Borrelia burgdorferi—in Australia and 'the diagnoses of [Australian] Lyme Borreliosis ... have
been primarily by clinical presentation and laboratory results of tentative
reliability and the true cause of these illnesses remains unknown'.[21]
2.26
However, patient advocacy groups and some medical practitioners
challenge this position and state that Borrelia bacteria known to cause
Lyme disease are endemic to Australia. These groups argue that Lyme disease is
a 'hidden epidemic' in Australia. They are concerned that there have been a
number of cases reported in the media of Australians who have been diagnosed
with Lyme disease acquired in Australia, but that these patients have been
'ignored' by the Australian health care system.[22]
2.27
In its submission, the Lyme Disease Association of Australia (LDAA)
suggests that evidence over the past fifty years that has demonstrated the
existence of an endemic species of Borrelia known to cause Lyme disease in
Australia has been 'systematically ignored' by medical authorities:
The presence of Borrelia, the causative agent of Lyme
disease, was established in Australian fauna in 1959 and human cases of Lyme
disease have been reported since the early eighties. Australian authorities
ignore this evidence.[23]
2.28
These groups highlight recent studies by Dr Peter Mayne, a retired NSW
medical practitioner, that suggest infection from B. burgdorferi has
been acquired in Australia by one patient and can be transmitted by Australian
ticks.[24]
However, the Communicable Diseases Network Australia has highlighted that the
absence of a published method to facilitate the replication of this finding
undermines its significance.[25]
2.29
Other groups, such as the Karl McManus Foundation, a charity that raises
funding for tick-borne disease research at the University of Sydney, assert
that the causative agent in Australia is not the same as classical Lyme disease
overseas, but an indigenous, Australian species of Borrelia:
...we do not have Borrelia burgdorferi, or Lyme disease,
in Australia. What we have is a unique Borrelia infection.[26]
2.30
The diagnostic procedures for testing for Borrelia bacteria in
Australia are examined in detail in Chapter 3.
Is an ongoing infection of Borrelia
bacteria responsible for chronic debilitating symptoms in Australian patients?
2.31
As noted in Chapter 1, the committee has heard that Australian
governments and medical authorities do not agree that the chronic debilitating
symptoms described by Australian patients are caused by an ongoing Borrelia
infection. These authorities assert that there is no evidence that the Borrelia
bacteria that cause Lyme disease are endemic to Australia and suggest that
there may be another as yet unidentified underlying cause or causes.[27]
2.32
For example, Professor Stephen Graves from the RCPA told the committee
that there is 'clearly something in Australian ticks, or some species of
Australian ticks, that is making some Australians sick',[28]
but it is unlikely to be caused by Borrelia:
I actually do not think what we are talking about is the Borrelia
infection. It is not classic Lyme disease. It is not a Borrelia
infection, although I am keeping an open mind on that possibility—but I do not
think it is. What is it?[29]
2.33
Dr Margaret Hardy, a research fellow at the University of Queensland's
Institute for Molecular Bioscience, told the committee that due to Australia's
geographic isolation, unique species of ticks and host animals, it is unlikely
that a Borrelia species similar to the Borrelia bacteria found in
North America and Europe would also be found in Australia:
America and Europe are much more geographically close as
well, so it would make sense that if you had two co-evolving types of Borrelia
you would see them across that close geographic range rather than coming all
the way up from there, missing Africa and Asia entirely, and popping up over in
Australia.[30]
2.34
Whereas Australian medical authorities suggest that the cause of the
chronic debilitating symptoms described by patients is not yet known, patient
advocacy groups assert that the cause is infection with Borrelia, together
with a range of other bacterial co-infections.[31]
These groups highlight that chronic Borrelia infection is just one of many
co-infections that are transmitted to humans by ticks and responsible for
causing chronic debilitating illness. For example, the LDAA submitted:
Emerging international research shows that Lyme disease is
rarely ever found in isolation of other pathogens; our research supports that
... Typically these are referred to as co-infections, but they are individual
and sometimes life threatening infections in their own right. As well as Borrelia,
an infection from each of those pathogens increases the complexity in the type
of symptoms patients actually endure.[32]
Tick-borne illnesses in Australia
2.35
The committee heard that due to the debate about Lyme disease, some
medical practitioners have limited awareness of other possible tick-borne
illnesses. A number of submitters reported that on presenting to their GP with
tick bites they were not offered any specific treatments and were told that
there are no tick borne illnesses in Australia. For example, Ms Linda Ebden
told the committee in Perth about her consultation with her GP:
I was covered in tick bites. He said to me: 'You have an
allergy. Go home and take some Phenergan.' I said to him, 'Is it possible that
it is something from the ticks?' He said, 'No, we do not have tick bite
diseases in Australia.' So I never learnt to protect myself. I thought being
bitten by ticks was just part and parcel of living in the hills.[33]
2.36
Ms Natalie Young, a National Parks Officer in NSW, noted in her
submission that she experienced over 300 tick bites over the course of her
career. As a result she suffered a range of debilitating symptoms including
headaches, fever, migratory pains and anxiety. Ms Young noted:
Doctor after doctor refused to acknowledge my large number of
tick bites as a causation of my illness even though I had had over 300 tick
bites at work over seven years. Local GP's were at a loss to explain my
illness. After I saw approximately ten local GP's, the referral process started
to specialists of varying fields. GP's were considering diagnoses of Chronic
Fatigue Syndrome, Tennis Elbow, Lupus, post-viral infections to Barmah and Ross
River Fever but as my disease severity worsened, they ruled these out.[34]
2.37
Whereas the committee acknowledges that there is significant debate
about whether or not Borrelia bacteria known to cause Lyme disease are
endemic to Australia, evidence to the committee suggests that both patient
advocacy groups and some medical authorities agree that there are likely to be
other pathogens in Australian ticks making people sick. Professor Peter
Collignon told the committee:
Ticks can cause lots of diseases, not only in Australia but
overseas. I think there are probably lots of organisms in ticks—bacteria and
even viruses—that we do not know of yet, so I think we have to keep an open
mind about what diseases may be transmitted by ticks and what therapy is available
or should be used for them.[35]
2.38
According to the department, there are 70 species of hard and soft ticks
in Australia, of which 16 species of hard ticks have been reported to bite
humans. The Paralysis Tick (Ixodes holocyclus) is understood to be
responsible for 95 per cent of tick bites in Eastern Australia.[36]
In Western Australia, a completely different species of tick, the ornate
kangaroo tick (Amblyomma triguttatum), is responsible for most tick bites
in humans.[37]
2.39
Ticks are hosts and vectors of a number of parasites, bacteria and
viruses. The main organisms that may be transmitted by ticks and associated
with disease known in Australia are outlined below:
-
Anaplasma – causes disease in cattle (bovine anaplasmosis,
or 'bovine tick fever') and dogs (canine anaplasmosis);
-
Babesia – a significant cause of disease in cattle (Bovine
babesiosis) and dogs (Canine babesiosis);[38]
-
Bartonella – causes disease in domestic and wild animals
including cats and kangaroos – uncertain whether it can cause human disease;
-
Ehrlichia – causes disease in dogs worldwide but has not
been recognised in Australia;
-
Francisella – relatively rare and no evidence to suggest
pathogenic for humans;
-
Rickettsia – causes several diseases in humans including
Queensland tick typhus (Rickettsia australis), Flinders Island spotted
fever (Rickettsia honei), variation of spotted fever (R. marmionii)
and Q fever (Coxiella burnetii – rarely tick-borne).[39]
2.40
The incidence of these tick-borne illnesses and their effects on
humans are not clearly known. A number of groups, including the RCPA, suggest
that further research needs to be undertaken into these other tick-borne
diseases and their impacts on humans.
Professor Stephen Graves told the committee:
Let us say it is bacteria, for argument's sake. Which one is
it? Or is it more than one? We cannot tell because we do not have the assays to
detect those bacteria or the antibodies produced in response to those bacteria
in the patients, because those assays have not been developed. That research
has not been done, and that is because the money has not been made available to
do it. Sorry to come back to money, but that is really what it takes ...
Someone has to look at Babesia and other protozoa that might be
responsible, and somebody has to look at viruses. In other parts of the world,
there are many viruses that are tick transmitted and cause very nasty diseases.
And we do not have one in Australia? Well, I cannot believe that. I cannot
believe that, senators. There have to be some viral tick-transmitted infections
in Australia; it is just that we do not know what they are.[40]
2.41
Both patient advocacy groups and medical authorities highlighted that
more research is needed into a range of key areas including identifying
possible pathogens in ticks and other vectors and clinical studies of patients.
These opportunities for research are examined in detail in Chapter 4.
2.42
A number of submitters and witnesses highlighted the need for better
education and awareness about preventing tick bites to avoid any potential
illnesses. Professor Peter Collignon told the committee:
We should avoid people being bitten by ticks. Ticks are bad
for lots of reasons, the same as mosquitos are really bad for people with, in
Australia, Ross River virus, Barmah Forest virus and a lot of things. So the
two insects that I think we should avoid being bitten by are ticks and
mosquitoes. I think we need to have a program to say what to do and,
particularly, how you remove a tick without causing more damage by squirting
more toxins or whatever into the person. So, yes, I think we need a tick
education program.[41]
2.43
The department noted in its submission that it is committed to education
and awareness raising about the prevention of tick bites and has produced a
publicly available information sheet on tick bites:[42]
In an effort to prevent tick-borne bites [sic] and raise
awareness of tick bite first aid, we collaborated with the National Arbovirus
and Malaria Advisory Committee as well as with states and territories on a tick
bite prevention document for public distribution. It is hoped in future we will
incorporate emerging research into tick bite associated mammalian meat allergy
and newer techniques for tick removal. The department is committed to such
education and awareness raising.[43]
Committee
view
2.44
The committee acknowledges that there is a debate about whether or not
Lyme disease is endemic to Australia. The committee notes the position of the
Chief Medical Officer that Lyme disease is not endemic to Australia as the
species of Borrelia bacteria responsible for causing the disease have
not been identified in Australia. The committee also notes evidence from Dr
Gary Lum that acknowledges that there may be another causative agent or agents
for the chronic debilitating illness described by patients.
2.45
The committee acknowledges that there may be illnesses transmitted by
ticks and potentially other vectors that warrant further research. The
committee notes that this issue needs further inquiry.
2.46
The committee recognises that more could be done to educate the public
and medical professionals about the risk of tick bites and tick-related
illnesses in Australia, as well as classical Lyme disease acquired overseas.
Treatment for patients diagnosed with Lyme-like illness
2.47
Patient advocacy groups argue that because Lyme disease is not
recognised as being endemic to Australia, patients seeking treatment experience
significant challenges accessing treatment.[44]
These difficulties include:
-
denial that someone is ill and denial of care;
-
stigma and humiliation associated with Lyme-like illness from some
medical services;
-
accessibility and costs of treatments prescribed by 'Lyme
literate practitioners'; and
-
limitations placed on 'Lyme literate' practitioners by medical
authorities.
Stigma and Lyme-like illness
2.48
Submitters expressed concern that because Lyme-like illness is not
recognised in Australia, patients experience significant stigma when seeking
treatment from some medical practitioners. These submitters note that medical
practitioners dismiss Lyme disease as a possible diagnosis, arguing that
Australia is not an endemic area and therefore Lyme disease does not exist
here.[45]
2.49
The committee notes that a large proportion of submitters to the inquiry
requested to have their submissions marked as either name withheld or
confidential to avoid any possible negative repercussions from their family,
friends, employers and medical practitioners.
2.50
One submitter described the treatment her 29 year old daughter had
received from medical professionals when she presented with Lyme-like illness:
The worst part of having this illness is the treatment and
discrimination that she has received by the majority of the medical profession.
She always had to justify why she was there and try to get them to understand
that she has pain, but after [a] brief discussion she would be told that there
is nothing medically wrong with her and her illness doesn't exist and that
stress is causing it all.[46]
2.51
Similarly, Ms Emily O'Sullivan, writing on behalf of her sister Amy, who
has been suffering chronic debilitating symptoms for 10 years and has been
diagnosed with Lyme-like illness, submitted that:
The Australian medical community not only fails to recognise
the disease but seem to have a proactive aversion to accepting Lyme Disease as
a possible diagnosis. This has left Amy in an unnerving cycle of denied care.
If she claimed to have Lyme Disease in GP clinics and ... hospitals (even with positive
blood tests), she was deemed 'crazy or looking for drugs' and didn’t receive
care because 'Lyme Disease doesn't exist in Australia'.[47]
2.52
The committee heard from a number of organisations representing patients
that indicated that patients are not treated with respect and care by some
medical practitioners. The LDAA noted in its submission that it receives:
... constant updates from Australians about how terribly they
are treated by the medical profession if they mention that they suspect or have
Lyme disease. Patient's [sic] routinely report poor treatment by Australian
GPs, infectious disease specialists and other hospital and specialist staff.[48]
2.53
The LDAA notes that the name 'Lyme disease' has attracted such a stigma
that 'many patients routinely advise others not to mention the disease at all
when reporting their medical history'.[49]
2.54
The committee is particularly concerned by evidence that suggests some
patients are humiliated or insulted by medical practitioners for seeking tests
or treatments for Lyme-like illness.[50]
The Australian Chronic Infectious and Inflammatory Disease Society (ACIIDS),
representing 'Lyme literate' practitioners, indicated that many patients have been
traumatised by some medical practitioners:
Discrimination against patients suffering from this illness,
and the doctors who treat them, is rife. Many patients have been traumatised by
their experience with medical specialists and in hospital emergency
departments; they have been subject to derision and verbal abuse.[51]
2.55
For example, one submitter described how their neurologist ridiculed
them when they brought up Lyme disease:
[My neurologist] spent a whole appointment ridiculing me and
asking me why I 'thought I had Lyme'. Repeating 'Lyme Disease is not in
Australia' [and] 'It can’t be Lyme Disease, we don't have Lyme in Australia'
[and] 'Show me proof it's here'[.]
I mentioned the paper that had just been realised [sic] from
Curtain [sic] University. This was found to have Borrelia on our native Fauna.
'That's on animals' he says.
So I leave another appointment in tears, frustrated and going
nowhere.[52]
2.56
One submitter, the father of a child with Lyme-like illness, said that
over three years of seeking treatment for his daughter the family faced a
series of refusals to treat and abuse by medical practitioners. During an
appointment with one neurologist, the family was subjected to a 'highly
abusive, emotional and irrational' outburst that included accusing the child of
feigning the symptoms and 'personal insults and attacks on the character' of
the child and their parents that 'deeply traumatised' the family.[53]
2.57
'Lyme literate' practitioners, such as Dr Richard Schloeffel, suggest
that the treatment of patients with Lyme-like illness by some medical
practitioners amounts to malpractice:
I cannot talk for other doctors and their thought processes,
but I would like to say to every doctor in Australia, 'Wake up to yourselves.
Start listening that we've got a real illness. Let's have a proper
conversation. Let's do the proper science. Let's fund it ... But we have to put
money into it, we have to have a proper conversation and the denialism has to
stop, because that is actually malpractice. It is actually negligence on the
part of the medical profession.[54]
2.58
Some medical authorities do not accept that there is any particular
stigma associated with Lyme disease or Lyme-like illness. For example, the
Australian Rickettsial Reference Laboratory submitted:
We do not accept that there is any more stigma associated
with "Lyme-like illness" than there is to many other medical
conditions from which many Australian patients already also suffer. Stigma,
where it exists, can be broken down by community education over time.
"Stigma" may be in the mind of the beholder. Some
patients may perceive that they are being stigmatised, but are probably not.
Their doctor is simply trying to obtain a diagnosis of their condition and
trying to treat the patient with the best of intentions and based on the
current state of medical knowledge. There are many patients who have an illness
that has not been currently diagnosed and for which there may be no recognised
treatment. Patients with "Lyme-like illness" are not the only
patients in this unfortunate position.[55]
2.59
Medical authorities noted that just because there is no evidence that
Lyme disease is endemic to Australia, it does not mean that doctors don't care
about the welfare of patients. Professor Samuel Zagarella told the committee:
When doctors say that Lyme disease does not exist in
Australia I think that a lot of people misinterpret that as being non-caring.
The question is whether these people are suffering from Lyme disease [or] a
different disease. We believe that at the moment there is no evidence to say
that they are suffering from Lyme disease caused by ticks, and caused by
Borrelia burgdorferi specifically. These people may be suffering from other
conditions. There are a lot of non-specific symptoms that these people suffer
from, such as arthritis, arthralgia, weakness, lethargy, pain and depression.
They certainly have some issues, but there is no evidence that Lyme disease as
such exists in Australia.[56]
Measures to reduce stigma
2.60
Some witnesses suggested that the stigma experienced by patients could
be reduced by avoiding use of the names 'Lyme disease' or 'Lyme-like illness'.
As noted in Chapter 1, submitters reported that they do not care what their
illness is called; they just want to be able to access treatment.
2.61
One alternative name suggested by Dr Lance Sanders is Hunter Valley
disease (HVD), in reference to the first documented case of a Lyme-like illness
reported in the Hunter Valley in the 1980s. Dr Sanders noted that this broad
term does not assume that the cause or causes for the symptoms have been
identified.[57]
2.62
In the United Kingdom, the name 'chronic arthropod-borne neuropathy' is
suggested by Dr Matthew Dryden to describe the range of symptoms experienced by
patients similar to those in Australia.[58]
2.63
Other possible names for the condition are advocated for by 'Lyme
literate' practitioners who argue that the symptoms are caused by Borreliosis
and a range of co-infections, such as US physician Dr Richard Horowitz.[59]
The name Multiple Systemic Infectious Disease Syndrome (MSIDS) is already used
by some patient advocacy groups in Western Australia in an attempt to move away
from the association with Lyme disease.[60]
2.64
Dr Lum told the committee that the department would support moving away
from the 'Lyme' label to better describe the 'chronic debilitating illness that
manifests as a constellation of chronic debilitating symptoms' described by
submitters:
We are well aware from the patient community and from various
members of the medical profession that moving right away from the notion of
Lyme disease and Lyme-disease-like illness is probably a very good move.
The problem that we have in Australia in terms of how we work
with patients, advocacy groups and the medical profession is that this is not
unique to Australia. The issue of a chronic Lyme disease is very contentious
and very controversial to the extent that we would like to steer away from
that. That is why in the work that we have been doing we have tried to
distinguish it by describing a chronic debilitating illness that manifests as a
constellation of chronic debilitating symptoms. That is a mouthful and I would
not propose that as a name. What I am trying to suggest though is that getting
away from that name is probably a very good move.[61]
2.65
Another measure to reduce stigma recommended by patients and advocacy
groups is formal recognition by Australian medical authorities of Lyme-like
illness.[62]
At its Brisbane hearing, the committee was presented with a 'Time to Recognise
Lyme' clock by Ms Karen Smith and Mr Matt Chant.[63]
Mr Chant told the committee:
The time to recognise Lyme clock is a call to action to show
that acknowledgement and treatment can help restore hope and health, that the
denial of Lyme and other vector borne diseases in Australia is causing
devastation and the loss of years of people's lives, and, in far too many
instances, their death.[64]
2.66
However, as noted in Chapter 1, Australian medical authorities do
not recognise Lyme-like illness as a defined condition, noting that it may be
used to describe a 'constellation of debilitating symptoms'.[65]
Committee
view
2.67
The committee is concerned by the treatment of patients diagnosed with
Lyme-like illness by some medical practitioners.
2.68
The committee notes that there are issues that need further inquiry,
such as:
-
ways to improve education and awareness about Lyme disease
acquired overseas;
-
ways to improve Australia's health care system to better meet the
needs of Australians with chronic illness; and
-
possible pathways for identifying an appropriate name and
definition for Lyme-like illness.
Accessibility and cost of treatment
2.69
A large number of patients diagnosed with Lyme-like illness expressed
concerns about the accessibility and high cost of treatments prescribed by
'Lyme literate' practitioners. 'Lyme literate' practitioners often prescribe a
course of treatment that may include antibiotics and other natural remedies
that are not supported by Medicare or the pharmaceutical benefits scheme (PBS).[66]
2.70
The committee heard that the cost of consulting 'Lyme literate'
practitioners is very expensive, with practitioners allegedly charging between
$300 and $900 for consultations.[67]
Diagnostic tests used by 'Lyme literate' practitioners also involve significant
expense (for example, $800 for tests in Australia and $2 000 for tests from
overseas laboratories).[68]
2.71
The treatments prescribed by 'Lyme literate' practitioners are also very
expensive, often costing hundreds of dollars per week. In one case, a submitter
claims to have spent over $100,000 on treatment since diagnosis.[69]
As a result of the high costs, a number of submitters, particularly those
receiving welfare or pension payments, note that they have not been able to
afford the prescribed treatments.[70]
For example, one submitter noted:
One drug for one of the coinfections alone costs over $1000
per month (and commonly needs to be taken for several months) but $6.10 if on
the PBS. This is just one example and most prescription treatments needed for
Lyme and coinfections are unsubsidized on the PBS so it is obvious that it
quickly becomes extremely costly to try to gain effective treatment for this
illness. The financial burden is enormous and I don't know what I'll do when I
run out of money.[71]
2.72
In some cases, submitters highlighted that some treatments prescribed by
'Lyme literate' doctors are not available in Australia. For example, submitters
have been referred to a clinic in Germany (Klinik St Georg in Bad Aibling) to
undertake 'hyperthermia treatment', where the body is heated to kill off
bacteria. This treatment is not available in Australia and costs approximately
$30 000 per course.[72]
Other submitters were referred to other similarly expensive treatments in the
US or elsewhere overseas (such as ozone therapy in Indonesia).[73]
2.73
As a result of these high costs, a number of submitters have highlighted
that they were experiencing significant financial hardship. Many submitters
reported having sold or mortgaged their homes, borrowed money from family and
friends or moved in with their parents or carers in order to afford treatments.[74]
2.74
Submitters have also highlighted that because Lyme-like illness is not formally
recognised, they have experienced difficulties in accessing social welfare
payments, income protection insurance and/or early access to superannuation to
pay for treatment and expressed concern and frustration that they did not
qualify for these payments and services.[75]
2.75
The department noted that to address the costs of treatments prescribed
by 'Lyme literate' practitioners, it would welcome an application for a review
of treatments to determine whether they could be included in the PBS:
...given the desire by patients and advocates for subsidised
pharmaceutical agents, the department would welcome a submission by the
advocacy groups to the Pharmaceutical Benefits Advisory Committee for a review
of the evidence.[76]
Appropriateness of treatments
2.76
The committee also heard concerns from medical authorities about some of
the treatments offered by 'Lyme literate' practitioners, such as side-effects
from antibiotics, infections from intravenous catheters (such as PICC lines)
and potential toxins from unregulated medications.[77]
These authorities argue that these treatments are not evidence based and risk
causing harm to patients.[78]
2.77
For example, one infectious disease specialist submitted:
I have been referred patients with Lyme disease, or such
patients have been referred to my colleagues. Sometime they already have
another diagnosis such as Motor Neurone Disease (MND). Then they are offered a
different diagnosis in a non-accredited lab, usually overseas. The lab is
usually not accredited in the overseas country and charges much more for tests
than mainstream labs ...
The patients are often given multiple diagnoses, none of
which are seen in Australia such as Babesiosis. In addition the treatment is
not standard, even were the diagnosis to be correct and invariably is for much
longer than in the IDSA (Infectious Diseases Society of America) guidelines. In
other words, even were the diagnosis to be correct the treatment is not
standard, and almost always has greater risks of side effects than conventional
treatment ...
The circumstances are not universal but there is a cluster of
patients diagnosed outside of medicine in un accredited [sic] laboratories and
given unorthodox treatment to the potentially severe detriment of their medical
and physical health as well as bearing a great financial and psychological
burden.[79]
2.78
In particular, the committee heard concerns about the use of long-term
antibiotics to address symptoms ascribed to Lyme-like illness. The Communicable
Diseases Network Australia, supported by state and territory health
departments, noted that:
There is no evidence to support the use of combination
antibiotics, immunoglobulin, hyperbaric oxygen, specific nutritional
supplements, or prolonged courses of antibiotics for the management of Lyme
disease.[80]
2.79
Associate Professor Samuel Zagarella from the Australasian College of
Dermatologists provided the committee with a recent study of a randomised trial
of long-term antibiotic therapy for symptoms attributed to Lyme disease in
Europe which concluded:
In patients with persistent symptoms attributed to Lyme
disease, longer-term antibiotic treatment did not have additional beneficial
effects on health-related quality of life beyond those with shorter-term
treatment.[81]
2.80
The RCPA further noted that the consequences of long-term antibiotic use
can have negative effects for both the individual and the broader community:
Unproven long term broad spectrum antibiotic treatment is not
only potentially harmful to the individual patient due to side-effects up to
and including death, it is harmful to the patient and the Australian community
in general because it promotes the proliferation of multi-drug resistant
organisms. This resistance renders all anti-biotics ineffective against common
(non-Lyme Disease) infections and is a genuine crisis in modern healthcare.[82]
2.81
However, 'Lyme literate' practitioners told the committee that the use
of long-term antibiotics was evidence based and in many cases assisted patients
to get better. Dr Richard Schloeffel, a Lyme literate practitioner in Sydney,
told the committee:
We have treated 4 000 patients in five years. We are
currently treating only 1 500 patients. Of the other 2 500 patients we have
treated, most are better. They are getting better because they are having an
appropriate diagnosis and appropriate treatment, sometimes with long-term
antibiotics—oral in the main. But because we have so many sick patients we are
doing a lot of intravenous therapies as well, including intravenous antibiotics
for long periods of time, which is leading to a positive outcome, but under the
same rigor that any intensive therapy would require, and we are doctors who are
extremely qualified to do this work.[83]
Committee
view
2.82
The committee notes that the following issues need further inquiry:
-
treatments prescribed for patients with Lyme-like illness,
including costs, efficacy and evidence base; and
-
the potential for a review of treatments by an expert panel.
Limitations on 'Lyme literate'
practitioners
2.83
Submitters expressed particular concern that 'Lyme literate'
practitioners experience stigma from medical authorities. In some cases,
practitioners have ceased providing treatment due to sanctions by or fear of
sanctions by medical authorities such as the Australian Health Practitioner
Regulation Agency (AHPRA). These submitters argue strongly that 'Lyme literate'
practitioners should not be prohibited from treating for Lyme-like illness.[84]
2.84
The committee notes that a number of practitioners who made submissions
to the inquiry requested that their name be withheld due to fear of
disciplinary action by AHPRA.[85]
Mr John Curnow, whose wife suffered from Lyme-like illness, noted in his
submission: 'The few doctors that do try to treat [this] Lyme like illness are
ostracised and called charlatans by their colleagues'.[86]
2.85
The LDAA also addressed this issue, noting that:
Of serious concern is the increasing level of complaints
being directed at doctors who are treating patients with Lyme disease. Over the
past three years there have been conditions placed on three doctors (Ladhams,
Du Preez and Kemp) treating patients with Lyme disease by the Australian Health
Practitioner Regulation Agency (AHPRA). The conditions are specific in response
to Lyme disease and relate to the diagnosis, treatment and prescribing
practices of the doctors concerned.[87]
2.86
According to the LDAA:
The small handful of doctors who are treating patients in
Australia are being bullied and badgered from within their profession and also
by AHPRA. It's probable that any Australian doctor that chooses to treat
Lyme-like disease will be investigated, given that they administer antibiotics
for a longer period of time than the one month treatment protocol and operate
outside the ATG's [Australian Therapeutic Guidelines].[88]
2.87
One doctor who made a submission to this inquiry noted that the effect
of such investigations was to constrain those doctors in their ability to treat
patients:
To my knowledge there are 7 medical practitioners who have
been 'targeted' for investigation and / or disciplinary measures. This makes
those of us willing to treat this condition fearful of such treatment.[89]
2.88
As a result of limitations placed on their practitioners by AHPRA, some
submitters noted that they were no longer able to get treatment. For example,
one submitter noted:
In 2013 I came under the care of a Lyme-literate doctor and
began receiving antibiotic treatment via a Portacath. I started to notice
changes quickly and then improvements within months...
In late 2013 my Lyme literate doctor faced disciplinary
action and was [told] he could no longer treat patients with Lyme disease. This
left me without a Lyme-literate doctor, or any doctor at all and with no access
to assistance with my Portacath for IV treatment. My husband rang many medical
centres in our local Redlands area and no one would help me.
As a result my health rapidly declined and I was dealing with
a Portacath that clotted and had no medical practitioner to assist with
flushing it. Thankfully my husband learned how to manage my Portacath with
videos that he found on YouTube.[90]
2.89
In response to this perception, representatives from AHPRA and the
Medical Board of Australia (MBA) told the committee at its Brisbane hearing that
AHPRA does not target Lyme-literate practitioners and only responds on the
basis of complaints:
... we recognise that there is a perception by some patients
that we have targeted medical practitioners who diagnose, treat or have a
relationship with Lyme-like illness. I would like to put it quite clearly on
the record that this is not true. In all the Lyme-related cases that we are or
have been involved with, the board has always acted—not in isolation or on its
own behalf—in response to a complaint.[91]
2.90
The Australian Medical Association (AMA) submitted that investigations
are initiated on the basis of specific complaints about the individual
practitioner:
The very small number of doctors who come before the MBA
often have a history of complaints made about them from the public and the
profession. The conditions imposed on the registration of any individual
medical practitioner are always specific to that practitioner. They do not
reflect the Board's view about any disease state or treatment regime. The AMA
continues to support the role of AHPRA and the MBA in this respect.[92]
2.91
Representatives from AHPRA and the MBA further stressed that in most
cases regarding Lyme literate practitioners, they have decided not to act. In
the small minority of cases where AHPRA does act, this is in response to the
professional conduct of the practitioners in question:
I would like to point out that in the majority of
notifications that have been in some way related with Lyme disease or Lyme in
some way, the board has decided not to act—not to act, to protect the public.
The matters have simply been investigated and then closed. It is in the small
number of cases where there is a greater risk, we perceive, to the public that
the board has taken a regulatory action to protect the public. It is on the public
record that we have received notifications about practitioners who have
diagnosed and treated Lyme disease. I would like to point out that it is not
because of the diagnosis that they are there before us, but because of their
professional conduct in the management of these patients. It is for these
patients that we have taken regulatory action.[93]
2.92
The MBA and AHPRA told the committee that in 2013-14 and 2014-15, of
complaints received relating to the treatment of Lyme-like symptoms:
-
9.3 per cent were made by medical practitioners (as mandatory
notifications under the Health Practitioner Regulation National Law); and
-
90.7 per cent were made by members of the public.[94]
2.93
The MBA and AHPRA listed some of the concerns related to Lyme disease or
Lyme-like illness which have led to an investigation of a medical practitioner:
-
the use of unconventional
diagnostic techniques (e.g. kinesiology) to diagnose Lyme-like disease;
-
the reliance on non-accredited
laboratories to diagnose Lyme-like disease;
-
the potential for financial
exploitation of patients, both through the use of overseas non-accredited
laboratories and in charging high fees for services;
-
not referring patients with
complex diagnoses to specialists, where this would have been appropriate;
-
not managing other co-existing
medical conditions once Lyme-like disease was diagnosed;
-
diagnosis of a large proportion of
a medical practitioner's patients with Lyme-like disease without considering or
excluding other conditions. There is a concern that patients may be deprived of
the opportunity to have more appropriate treatment for another condition
because the alternative condition is not considered once Lyme-like illness has
been diagnosed. Treating Lyme-like illness with long-term antibiotic treatment,
in the absence of an identified infection, is of concern. This management is at
odds with advice from public health authorities regarding the dangers of
antibiotic resistance. We understand that some practitioners are prescribing
and administering antibiotics for years (whereas the treatment of Lyme disease
is for weeks); and
-
treatment for Lyme-like disease
resulting in complications and interacting or interfering with other
treatments. Examples include, use of large lines (e.g. PICC lines) to
administer long-term antibiotics, which can result in infections and
thrombosis, and antibiotics interacting with other necessary treatments.[95]
2.94
The committee heard that AHPRA and the MBA have not considered ways to
communicate decisions about 'Lyme literate' practitioners to other practitioners
and the patient community. At the suggestion of the committee that this be
considered, Associate Professor Stephen Bradshaw from AHPRA told the committee:
To be honest with you, we have not considered what you have
just suggested. We may consider that after. I re-emphasise to you that we are
not a disease-focused organisation—be it Lyme disease, cancer or whatever. We
are looking for good medical practice. It is disappointing that there is this
perception out there that we are targeting particular groups; I re-emphasise
and will keep re-emphasising that we certainly are not. At the end of the day,
the number of practitioners that have regulatory action taken against them on
this topic is extremely small. There are huge other areas of practice that have
a lot more practitioners before us than practitioners looking after patients
with Lyme disease.[96]
Navigation: Previous Page | Contents | Next Page